Estimating the Role of Air Quality Improvements in the Decline of Suicide Rates in China
Improvements in air quality have coincided with declining suicide rates in many regions of the globe, yet whether the two phenomena are causally linked has yet to be uncovered. In this study, the authors use comprehensive data from across Chinese counties to show that suicide rates increase substantially when air pollution rises, and that older women are far more vulnerable than other groups. China’s recent “war on pollution” is estimated to have prevented 46,000 suicide deaths across the country in just five years, explaining 10% of the overall decline in suicide rates over 2013–2017.

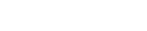
Suicide is a leading cause of death in multiple countries, representing a stark indicator of extensive mental health challenges in many parts of the globe. However, there is room for optimism: in recent years, a downtrend in reported suicide rates has emerged globally. From 2000 to 2019, the WHO estimates that the global average suicide rate decreased by about 16%, with particularly large declines in low- and middle-income countries, where 80% of global suicides occur (WHO 2021). China, home to nearly 20% of global suicides, is estimated to have seen the most dramatic suicide rate decline of any nation on earth (Figure 1). While the economic, social, and cultural factors contributing to this improvement have been previously investigated, the potential role of changing environmental conditions in shaping suicide risk in China has yet to be uncovered.
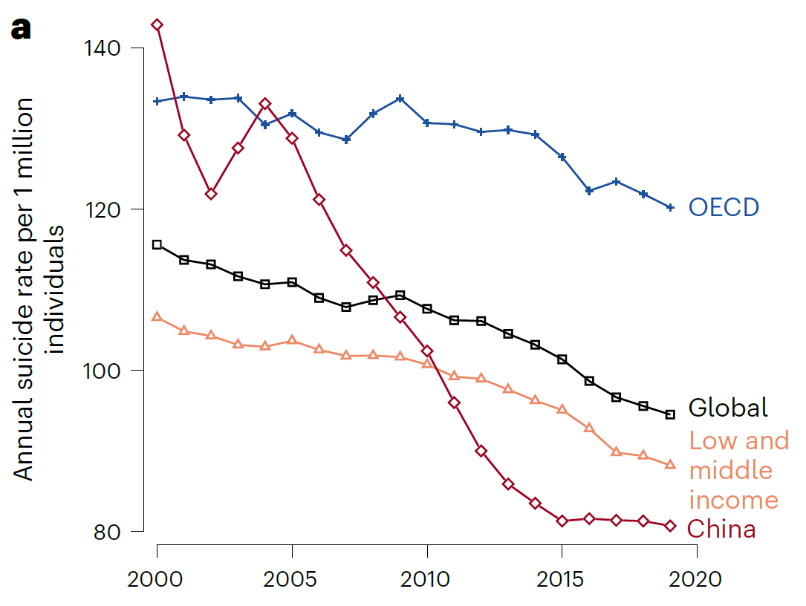
Figure 1. Declining suicide rates across the globe. Time series of annual average suicide rates globally (black), for the OECD (blue), low- and middle-income countries (orange) and China (red). Unweighted averages are shown using annual country-level data from WHO (2021).
One salient environmental factor that may contribute to suicide rate declines in China is air pollution. A growing body of research has unveiled a strong correlational relationship between air pollution and suicide (Changsoo Kim et al. 2010; Lin et al. 2016; Yoonhee Kim et al. 2018; Braithwaite et al. 2019; Davoudi et al. 2021; Heo, Lee, and Bell 2021), and air quality has markedly improved in recent years across China (Greenstone et al. 2021). These studies suggest various underlying pathways. First, particulate matter neurologically impacts brain function through the modulation of serotonin release (Pandey 2013; Ragguett et al. 2017; Heo, Lee, and Bell 2021). Second, the adverse effects of air pollution on physical health, such as cardiovascular and respiratory diseases, subsequently impact mental well-being (Brunekreef et al. 2002; Filik et al. 2006; Collins, Tranter, and Irvine 2012). Third, the negative influence of air pollution on economic productivity and output could potentially impact economically motivated suicides (Graff Zivin and Neidell 2012; Fu, Viard, and Zhang 2021; Carleton 2017).
However, isolating the role of air pollution from the many other cultural, social, and economic factors driving suicide is incredibly difficult, as the factors often correlate with the activities that generate air pollution (Braithwaite et al. 2019). No countrywide analyses tackling this challenge exist, particularly for China.
To fill this gap, we match the data from over 139,000 weekly reports on suicides across 597 representative counties in China from 2013 to 2017 with reports from about 1,400 air pollution monitors throughout the country. During the sample period, air pollution levels and suicide rates show consistent seasonal changes and overall reductions. To estimate the causal impact of pollution on suicide rates, we employ instrumental variables regression within a panel data framework, which helps us separate the impact of pollution from other factors, such as changes in economic activity, cultural norms, or physical health. Specifically, we use climatological events called thermal inversions, which flip the standard negative altitudinal temperature gradient and trap air pollution near the Earth’s surface, to isolate plausibly random variation in on-the-ground pollution exposure. These events occur when there is a rapid cooling of the Earth’s surface during clear, cold nights with minimal wind, when vertical air movements cause cold air to descend rapidly, or when layers of air at different temperatures move horizontally in warm or cold fronts (Jacobson 2002). This strategy has been used to identify the impact of air pollution on other outcomes, such as physical health (Arceo, Hanna, and Oliva 2016) and economic productivity (Chen, Oliva, and Zhang 2022).
Our analysis reveals that thermal inversions are robust indicators of PM2.5 levels across Chinese counties. On average, the occurrence of one additional inversion per week corresponds to a rise in weekly county-level PM2.5 by approximately 0.51 μg m−3 (±0.08, with the range indicating ±1 s.e.), constituting approximately 1% of the sample.
Using thermal inversions as an instrumental variable for PM2.5, we estimate that a one s.d. increase in PM2.5 leads to a rise in weekly suicide rates of 0.24 (±0.09) per 1 million individuals, representing an approximately 25% increase above the average weekly suicide rate (Figure 2). This coefficient demonstrates high statistical significance, as indicated by a corresponding p-value of 0.006. In contrast, employing linear regression without an instrumental variable (often referred to as a two-way fixed effects regression) yields a small and statistically insignificant estimate of the suicide–PM2.5 relationship, which aligns with prior literature. The intuition behind this bias is that much of the activity generating pollution, such as elevated economic production, heavy commuting traffic, and high demands on power plants, is associated with favorable economic conditions, which lower suicide risk (Cai et al. 2022). In statistical analyses that cannot separate the role of pollution from these economic factors, recovered coefficients are likely to be downward biased.
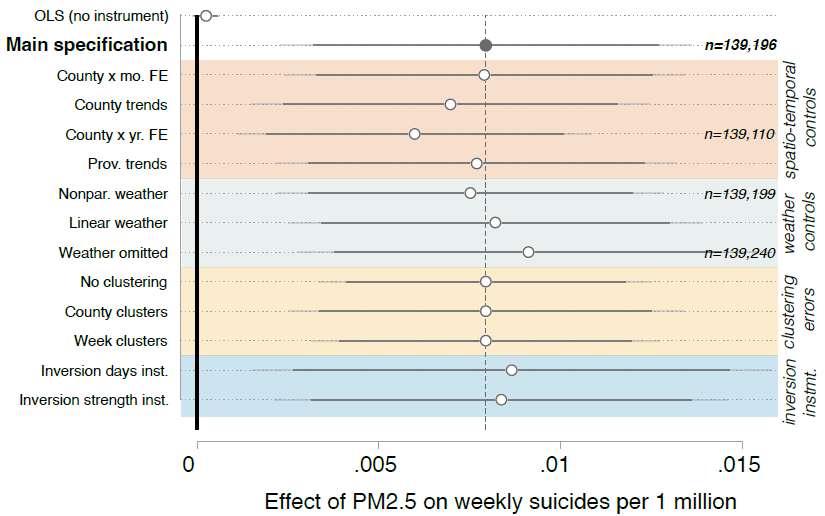
Figure 2. Estimated effects of air pollution on suicide rates in China. Estimated effect of a 1 μgm−3 increase in PM2.5 on the suicide rate per 1 million individuals. The top row shows a correlational relationship between suicide rates and PM2.5, estimated using a two-way fixed-effects model. The main specification in the second row uses thermal inversions to the instrument for PM2.5. Other estimates below show the robustness of the instrumental variable approach.
We show that this effect of air pollution on suicide differs strongly across subpopulations in China. Particularly, the oldest age group—individuals aged 65–85 years—are far more susceptible compared to other age cohorts. Specifically, our findings highlight a pronounced vulnerability among older females, who exhibit a far greater susceptibility to PM2.5 compared to males (Figure 3). For women aged 65–85, the suicide rate increases by 63% per standard deviation rise in air pollution. Effects of air pollution are also higher in counties with high baseline suicide rates, possibly indicating “suicide contagion” effects where a suicide in a given community can raise the risk of suicide for other members of the community.
Figure 3. Heterogeneity in the effect of PM2.5 on the suicide rate. The point estimate and associated confidence intervals for the main specification are shown in gray. All other estimates use subsamples of the data, splitting by age and sex (orange), season of the year (yellow), county-level urban and rural designation (green), wealthiest 15 provinces and all others (light blue), terciles of sample average PM2.5 (blue), and terciles of average suicide rate (navy).
Various mechanisms linking suicide and PM2.5 are likely to unfold over different time scales. Our analysis reveals that suicide rates exhibit a very rapid response to climatic conditions that elevate PM2.5 levels: weekly suicide rates increase in the same week that thermal inversions raise pollution (Figure 4). Interestingly, there is no discernible effect of thermal inversions on suicides even one week into the future. These findings suggest that a direct neurobiological mechanism is at play, as opposed to a channel for suicide risk through pollution-induced physical health or economic productivity effects. Such a rapid response is consistent with previous neurobiological and epidemiological literature, which repeatedly uncovered acute effects, in which near-immediate impacts of air pollution on respiratory, cardiovascular, and/or neurological functioning elevate suicide risk (Davoudi et al. 2021; Ragguett et al. 2017). For example, particulate matter can change brain chemistry, altering aggression and emotional control within 24 hours (Biermann et al. 2009). Similarly, air pollutants impact brain-derived neurotropic factor rapidly, very quickly affecting an individual’s ability to cope with crises (Ragguett et al. 2017). Experimental studies show that human neuronal cell death increases within 72 hours of exposure to PM2.5 (Wei et al. 2017).
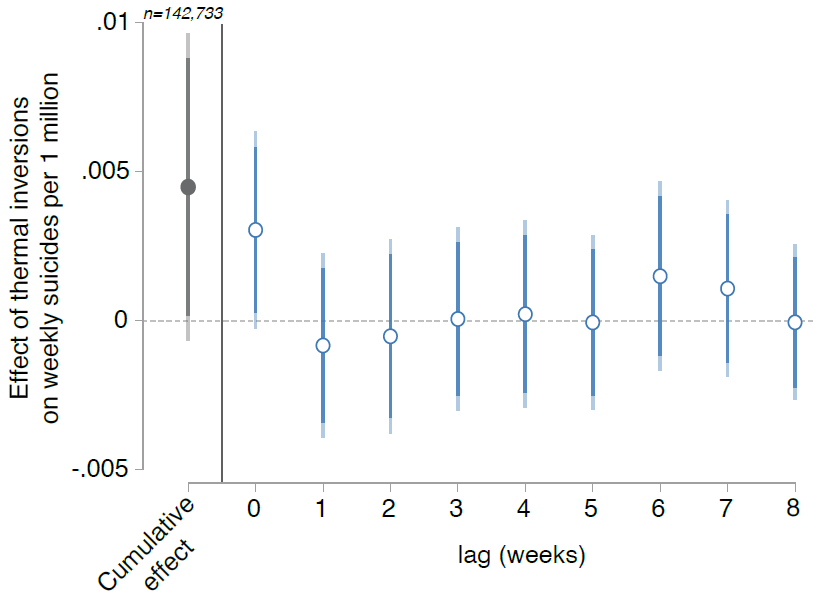
Figure 4. Dynamic effect of thermal inversions on the suicide rate. The cumulative effect represents the total effect of inversions on suicide rates over eight weeks; individual lagged effects indicate the effect of contemporaneous (lag zero) thermal inversions and those up to eight weeks.
Using these findings and nationwide pollution data, we compute county- and year-specific estimates of the reduction in suicide deaths attributable to changes in PM2.5 levels since 2013, the implementation year of China’s Air Pollution Prevention and Control Action Plan (Figure 5). Our analysis suggests that improvements in PM2.5 levels across China during the period from 2013 to 2017 averted an estimated 45,970 (±16,712) suicides. Notably, we find that PM2.5 improvements in specific districts resulted in substantial reductions in suicide deaths. For instance, in Pudong New District, a district of Shanghai, approximately 155 suicides (±56) were prevented over the course of five years. Similarly, in Binhai, a district of Tianjin, and Wuhou, a district of Chengdu, an estimated 122 (±44) and 106 (±39) suicides, respectively, were prevented. These findings underscore the significant public health benefits associated with improvements in air quality and highlight the potential for targeted interventions to mitigate suicide risk, particularly in areas experiencing rapid industrialization and urbanization.

Figure 5. Prevented suicides attributable to recent pollution declines. Estimates of suicides prevented by observed declines in PM2.5 between 2013 and 2017 for 2,500 Chinese counties. Prefectures are outlined in light gray and provinces in dark gray. Solid gray regions indicate areas with no available population and/or PM2.5 data.
In conclusion, China has witnessed a consistent decline in suicide rates in recent years, possibly due to factors like rising incomes, cultural shifts, and lower lethality of pesticides used in agriculture. While there is growing evidence to suggest that air pollution reduction might also play a role, its specific impact hasn’t been fully explored in extant literature. By employing instrumental variable regression, we find that approximately 10% of China’s recent decrease in suicide rates can be attributed to PM2.5 improvements. Despite various socioeconomic and demographic shifts influencing suicide rates, our study highlights air pollution as a significant contributing factor, adding urgency to calls to clear the skies across the globe.
References
Arceo, Eva, Rema Hanna, and Paulina Oliva. 2016. “Does the Effect of Pollution on Infant Mortality Differ between Developing and Developed Countries? Evidence from Mexico City.” Economic Journal 126 (591): 257–80. https://doi.org/10.1111/ecoj.12273.
Astudillo-García, Claudia Iveth, Laura Andrea Rodríguez-Villamizar, Marlene Cortez-Lugo, Julio César Cruz-De la Cruz, and Julián Alfredo Fernández-Niño. 2019. “Air Pollution and Suicide in Mexico City: A Time Series Analysis, 2000–2016.” International Journal of Environmental Research and Public Health 16 (16): 2971. https://doi.org/10.3390/ijerph16162971.
Bakian, Amanda V., Rebekah S. Huber, Hilary Coon, Douglas Gray, Phillip Wilson, William M. McMahon, and Perry F. Renshaw. 2015. “Acute Air Pollution Exposure and Risk of Suicide Completion.” American Journal of Epidemiology 181 (5): 295–303. https://doi.org/10.1093/aje/kwu341.
Biermann, Teresa, Nikolaos Stilianakis, Stefan Bleich, Norbert Thürauf, Johannes Kornhuber, and Udo Reulbach. 2009. “The Hypothesis of an Impact of Ozone on the Occurrence of Completed and Attempted Suicides.” Medical Hypotheses 72 (3): 338–341. https://doi.org/10.1016/j.mehy.2008.09.042.
Braithwaite, Isobel, Shuo Zhang, James B. Kirkbride, David. P. J. Osborn, and Joseph F. Hayes. 2019. “Air Pollution (Particulate Matter) Exposure and Associations with Depression, Anxiety, Bipolar, Psychosis and Suicide Risk: A Systematic Review and Meta-analysis.” Environmental Health Perspectives 127 (12): 126002. https://doi.org/10.1289/EHP4595.
Brunekreef, Bert, and Stephen T. Holgate. 2002. “Air Pollution and Health.” Lancet 360 (9341): 1233–42. https://doi.org/10.1016/S0140-6736(02)11274-8.
Cai, Ziyi, Mengni Chen, Pengpeng Ye, and Paul S. F. Yip. 2022. “Socio-economic Determinants of Suicide Rates in Transforming China: A Spatial-Temporal Analysis from 1990 to 2015.” Lancet Regional Health Western Pacific 19: 100341. https://doi.org/10.1016/j.lanwpc.2021.100341.
Carleton, Tamma A. 2017. “Crop-Damaging Temperatures Increase Suicide Rates in India.” Proceedings of the National Academy of Sciences of the United States of America 114 (33): 8746–51. https://doi.org/10.1073/pnas.1701354114.
Casas, Lidia, Bianca Cox, Mariska Bauwelinck, Benoit Nemery, Patrick Deboosere, and Tim Steve Nawrot. 2017. “Does Air Pollution Trigger Suicide? A Case-Crossover Analysis of Suicide Deaths over the Life Span.” European Journal of Epidemiology 32 (11): 973–81. https://doi.org/10.1007/s10654-017-0273-8.
Chen, Shuai, Paulina Oliva, and Peng Zhang. 2022. “The Effect of Air Pollution on Migration: Evidence from China.” Journal of Development Economics 156: 102833. https://doi.org/10.1016/j.jdeveco.2022.102833.
Collins, Eve, Siobhan Tranter, and Fiona Irvine. 2012. “The Physical Health of the Seriously Mentally Ill: An Overview of the Literature.” Journal of Psychiatric and Mental Health Nursing 19 (7): 638–46. https://doi.org/10.1111/j.1365-2850.2011.01831.x.
Davoudi, Mojtaba, Fateme Barjasteh-Askari, Homayoun Amini, David Lester, Amir Hossein Mahvi, Vahid Ghavami, and Mohammad Rezvani Ghalhari. 2021. “Association of Suicide with Short-Term Exposure to Air Pollution at Different Lag Times: A Systematic Review and Meta-analysis.” Science of the Total Environment 771, 144882. https://doi.org/10.1016/j.scitotenv.2020.144882.
Filik, Rachel, Atilla Sipos, Patrick Kehoe, T. Burns, S. J. Cooper, H. Stevens, R. Laugharne, G. Young, S. Perrington, J. McKendrick, D. Stephenson, and G. Harrison. 2006. “The Cardiovascular and Respiratory Health of People with Schizophrenia.” Acta Psychiatrica Scandinavica 113, 298–305. https://doi.org/10.1111/j.1600-0447.2006.00768.x.
Fu, Shihe, V. Brian Viard, and Peng Zhang. 2021. “Air Pollution and Manufacturing Firm Productivity: Nationwide Estimates for China.” Economic Journal 131, 3241–73. https://doi.org/10.1093/ej/ueab033.
Graff Zivin, Joshua, and Matthew Neidell. 2012. “The Impact of Pollution on Worker Productivity.” American Economic Review 102 (7): 3652–73. https://doi.org/10.1257/aer.102.7.3652.
Greenstone, Michael, Guojun He, Shanjun Li, and Eric Yongchen Zou. 2021. “China’s War on Pollution: Evidence from the First 5 Years.” Review of Environmental Economics and Policy 15 (2): 281–99. https://doi.org/10.1086/715550.
Heo, Seulkee, Whanhee Lee, and Michelle L. Bell. 2021. “Suicide and Associations with Air Pollution and Ambient Temperature: A Systematic Review and Meta-analysis.” International Journal of Environmental Research and Public Health 18 (14): 7699. http://dx.doi.org/10.3390/ijerph18147699.
Jacobson, Mark Z. 2002. Atmospheric Pollution: History, Science, and Regulation. Newcastle upon Tyne, UK: Cambridge University Press.
Kim, Changsoo, Sang Hyuk Jung, Dae Ryong Kang, Hyeon Chang Kim, Ki Tae Moon, Nam Wook Hur, Dong Chun Shin, and Il Suh. 2010. “Ambient Particulate Matter as a Risk Factor for Suicide.” American Journal of Psychiatry 167 (9): 1100–1107. https://doi.org/10.1176/appi.ajp.2010.09050706.
Kim, Yoonhee, Chris Fook Sheng Ng, Yeonseung Chung, Ho Kim, Yasushi Honda, Yue Leon Guo, Youn-Hee Lim, Bing-Yu Chen, Lisa A. Page, and Masahiro Hashizume. 2018. “Air Pollution and Suicide in 10 Cities in Northeast Asia: A Time-Stratified Case-Crossover Analysis.” Environmental Health Perspectives 126 (3): 037002. https://doi.org/10.1289/EHP2223.
Lee, Hyewon, Woojae Myung, Satbyul Estella Kim, Doh Kwan Kim, and Ho Kim. 2018. “Ambient Air Pollution and Completed Suicide in 26 South Korean Cities: Effect Modification by Demographic and Socioeconomic Factors.” Science of the Total Environment 639: 944–51. https://doi.org/10.1016/j.scitotenv.2018.05.210.
Lin, Guo-Zhen, Li Li, Yun-Feng Song, Ying-Xue Zhou, Shuang-Quan Shen, and Chun-Quan Ou. 2016. “The Impact of Ambient Air Pollution on Suicide Mortality: A Case-Crossover Study in Guangzhou, China.” Environmental Health 15, 90. https://doi.org/10.1186/s12940-016-0177-1.
Ng, Chris Fook Sheng, Andrew Stickley, Shoko Konishi, and Chiho Watanabe. 2016. “Ambient Air Pollution and Suicide in Tokyo, 2001–2011.” Journal of Affective Disorders 201: 194–202. https://doi.org/10.1016/j.jad.2016.05.006.
Pandey, Ghanshyam N. “Biological Basis of Suicide and Suicidal Behavior.” 2013. Bipolar Disorders 15 (5): 524–41. http://dx.doi.org/10.1111/bdi.12089.
Ragguett, Renee-Marie, Danielle S. Cha, Mehala Subramaniapillai, Nicole E. Carmona, Yena Lee, Duanduan Yuan, Carola Rong, and Roger S. McIntyre. 2017. “Air Pollution, Aeroallergens, and Suicidality: A Review of the Effects of Air Pollution and Aeroallergens on Suicidal Behavior and an Exploration of Possible Mechanisms.” Review of Environmental Health 32 (4): 343–59. https://doi.org/10.1515/reveh-2017-0011.
Wei, Hongying, Yan Feng, Fan Liang, Wei Cheng, Xiaomeng Wu, Ren Zhou, Yan Wang. 2017. “Role of Oxidative Stress and DNA Hydroxymethylation in the Neurotoxicity of Fine Particulate Matter.” Toxicology 380: 94–103. https://doi.org/10.1016/j.tox.2017.01.017.
World Health Organization. 2021. Suicide Worldwide in 2019: Global Health Estimates. https://www.who.int/publications/i/ item/9789240026643.

Latest
Most Popular
- VoxChina Covid-19 Forum (Second Edition): China’s Post-Lockdown Economic Recovery VoxChina, Apr 18, 2020
- China’s Great Housing Boom Kaiji Chen, Yi Wen, Oct 11, 2017
- China’s Joint Venture Policy and the International Transfer of Technology Kun Jiang, Wolfgang Keller, Larry D. Qiu, William Ridley, Feb 06, 2019
- The Dark Side of the Chinese Fiscal Stimulus: Evidence from Local Government Debt Yi Huang, Marco Pagano, Ugo Panizza, Jun 28, 2017
- Wealth Redistribution in the Chinese Stock Market: the Role of Bubbles and Crashes Li An, Jiangze Bian, Dong Lou, Donghui Shi, Jul 01, 2020
- What Is Special about China’s Housing Boom? Edward L. Glaeser, Wei Huang, Yueran Ma, Andrei Shleifer, Jun 20, 2017
- Evaluating Risk across Chinese Housing Markets Yongheng Deng, Joseph Gyourko, Jing Wu, Aug 02, 2017
- Privatization and Productivity in China Yuyu Chen, Mitsuru Igami, Masayuki Sawada, Mo Xiao, Jan 31, 2018
- How did China Move Up the Global Value Chains? Hiau Looi Kee, Heiwai Tang, Aug 30, 2017
- China’s Shadow Banking Sector: Wealth Management Products and Issuing Banks Viral V. Acharya, Jun Qian, Zhishu Yang, Aug 09, 2017



 Facebook
Facebook  Twitter
Twitter  Instagram
Instagram WeChat
WeChat  Email
Email